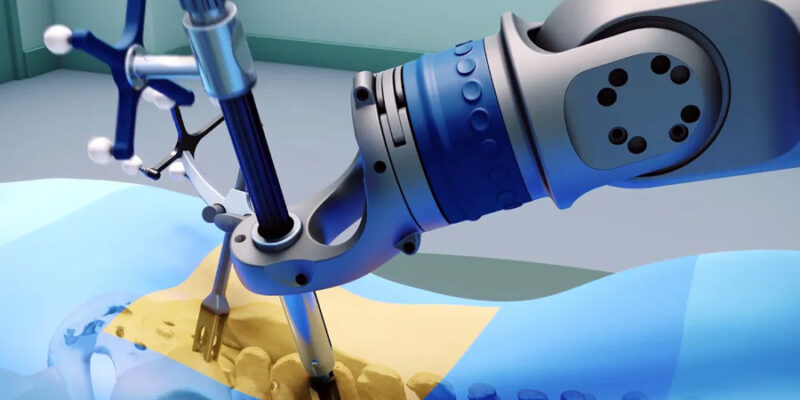
Multilevel spinal disc replacement is a complex surgical procedure that involves replacing more than one degenerated disc in the spinal column, often in the cervical or lumbar regions. These surgeries are highly technical and require an in-depth understanding of spinal biomechanics, patient anatomy and long-term functional goals. Dr. Larry Davidson, an experienced surgeon in the field, recognizes that success in multilevel disc replacement hinges on careful preoperative planning. Data modeling is emerging as a key tool for enhancing surgical decision-making.
Data modeling allows surgeons to simulate outcomes, predict potential complications and fine-tune implant selection based on individual patient variables. Using Artificial Intelligence (AI) and machine learning, these models integrate vast amounts of clinical data to help spine specialists make more precise and confident choices in surgical planning and execution. For patients undergoing multilevel disc replacement, this means more personalized care and better long-term results.
Understanding the Challenges of Multilevel Disc Replacement
Unlike single-level procedures, multilevel disc replacement comes with added complexity. Surgeons must account for the interaction between multiple spinal segments, evaluate load distribution across the spine and determine the optimal number and location of artificial discs. Even a small miscalculation in spacing or alignment can affect spinal stability and lead to long-term complications such as implant wear, adjacent segment degeneration or altered mobility.
In addition, patient-specific factors, such as existing spinal curvature, bone density, muscle strength and medical history, play a significant role in determining which approach and implant type will provide the best outcome. Traditional planning tools are often insufficient to process this level of detail, making data modeling a crucial advancement in surgical planning.
What Is Data Modeling in Spine Surgery?
Data modeling in spinal surgery uses patient imaging and records to simulate spinal biomechanics and predict treatment outcomes. It helps surgeons assess how different procedures and implants will perform, especially in complex cases like multilevel disc replacement, where decisions affect multiple vertebrae.
Personalized Surgical Planning Through Predictive Simulations
Data modeling enables personalized surgical plans by analyzing scans and factors like age, activity level and spinal conditions. In complex cases, AI can simulate various treatment paths and suggest the most effective strategy to maintain spinal alignment and minimize stress, ensuring care is personalized rather than one-size-fits-all.
Selecting the Right Implant Combinations
Selecting the right disc combination for multilevel procedures is complex, as not all designs work well together. By analyzing how implants move, interact with surrounding structures and respond to stress, data modeling creates side-by-side simulations that guide surgeons toward the best possible implant choice.
Anticipating Long-Term Biomechanical Outcomes
One of the most powerful benefits of data modeling is its ability to predict long-term outcomes. These simulations evaluate how the spine will respond to implant placement over time, including wear patterns, stress distribution and the potential for adjacent segment degeneration. These insights help surgeons plan for longevity, not just immediate results.
Reflecting on recent advancements, Dr. Larry Davidson shares, “If the progress we’ve seen in just the past decade is any indication, the future holds even more remarkable innovations, not only in surgical techniques, but also in the technologies that support spine surgeons in achieving better outcomes. It’s hard not to feel inspired by what lies ahead.” His optimism echoes the growing role of data modeling in surgical planning, where technology is increasingly used to make patient-centered decisions with long-term results in mind.
Anticipating these biomechanical changes is critical in multilevel disc replacement. A poorly chosen strategy might temporarily relieve pain but lead to hardware failure or further degeneration down the line. Data modeling offers a clearer picture of what to expect over the years, guiding more sustainable surgical decisions.
Reducing Revision Surgery Rates
Revision surgeries are particularly complex and risky in multilevel procedures. By using data modeling to get the plan right the first time, surgeons can significantly reduce the likelihood of revision due to implant misalignment, suboptimal disc choice or unexpected wear.
Studies have shown that the integration of predictive models into surgical planning helps reduce complications and improve surgical accuracy. With fewer post-operative issues, patients recover faster and experience fewer disruptions to their lifestyle and mobility.
Enhancing Collaboration Within the Surgical Team
Data modeling enhances not only the surgeon’s planning process but also collaboration across the broader care team. Simulations can be shared with radiologists, anesthesiologists, physical therapists and even implant manufacturers to ensure everyone is aligned on strategy and execution. This is particularly critical in multilevel procedures, where precision and coordination are essential. With a unified, data-informed approach, teams can work from a shared understanding of patient goals and procedural complexity.
Educating and Empowering Patients
Data modeling platforms often include visualization tools that help explain surgical plans to patients. Rather than relying on abstract descriptions, surgeons can show patients how their spine currently functions and how the replacement will improve movement or stability.
This transparency builds trust and enhances patient engagement. When individuals understand the reasoning behind their treatment plan and see how the choices are based on real data, they’re more likely to commit to recovery protocols and follow-up care.
Limitations and Continued Development
Like any evolving technology, data modeling comes with its limitations. The accuracy of its simulations hinges on the depth and diversity of the data used to train its algorithms. When rare anatomical variations or less common conditions aren’t well represented, the model’s ability to predict outcomes can be affected.
Nonetheless, continued research and model refinement are helping expand the utility of data modeling across more spinal conditions and populations. As data becomes more comprehensive and AI systems more adaptive, these models will only grow stronger in predictive value and clinical relevance.
Smarter Surgeries for Better Spinal Health
As spinal disc replacement evolves, data modeling is becoming an essential part of the decision-making process, especially in multilevel cases. From implant selection to motion simulations and long-term outcome forecasts, these tools bring a level of precision and personalization that was once impossible.
With data-driven insights guiding surgical choices, spine specialists are better equipped to deliver optimal outcomes. For patients, it means a smoother recovery, longer-lasting results and the ability to return to life with greater confidence and mobility.
As predictive modeling continues to improve, multilevel spinal disc replacement is shifting from a high-stakes procedure into one guided by foresight, collaboration and customization. It represents a smarter path forward, where advanced planning and clinical expertise come together to support better care, fewer complications and stronger long-term quality of life.











Comments